Whilst most people associate scoliosis with children or teenagers, scoliosis can actually develop – particularly after the age of 40 – and it is more common than many people realise. The good news is that learning how to manage it early can help reduce its impact and support long-term spinal health.
What is scoliosis?
Scoliosis is a condition where the spine curves sideways in an “S” or “C” shape. The degree of curvature can vary from mild and barely noticeable to more pronounced – doctors can measure the curvature of the spine to determine the impact the changes may have. While many cases of scoliosis develop during adolescence, adult-onset or degenerative scoliosis can develop later in life.
Why does scoliosis develop with age?
As we get older, the discs and joints in the spine naturally begin to wear down. When this degeneration occurs unevenly, the spine may start to lose its normal alignment and begin to curve. Ageing is also associated with sarcopenia – a gradual loss of muscle mass – and a decline in bone density, which can lead to conditions like osteopenia or osteoporosis.
Although these changes affect both men and women, they tend to be more pronounced in women during and after menopause. This is largely due to the drop in oestrogen levels, which plays a key role in maintaining healthy bones and strong, supportive muscles. When bone strength and muscular support are compromised, the spine becomes more vulnerable to developing abnormal curvatures and posture-related changes. These same changes will also contribute to potential worsening of existing scoliotic curves in older age.
The impact of scoliosis
Over time, a changing spinal position can lead to a range of symptoms. These may include joint stiffness, pain, and muscle imbalances that make some areas feel overworked or tight. In more advanced cases, compression in the spinal joints can affect nearby nerves – potentially leading to issues like sciatica.
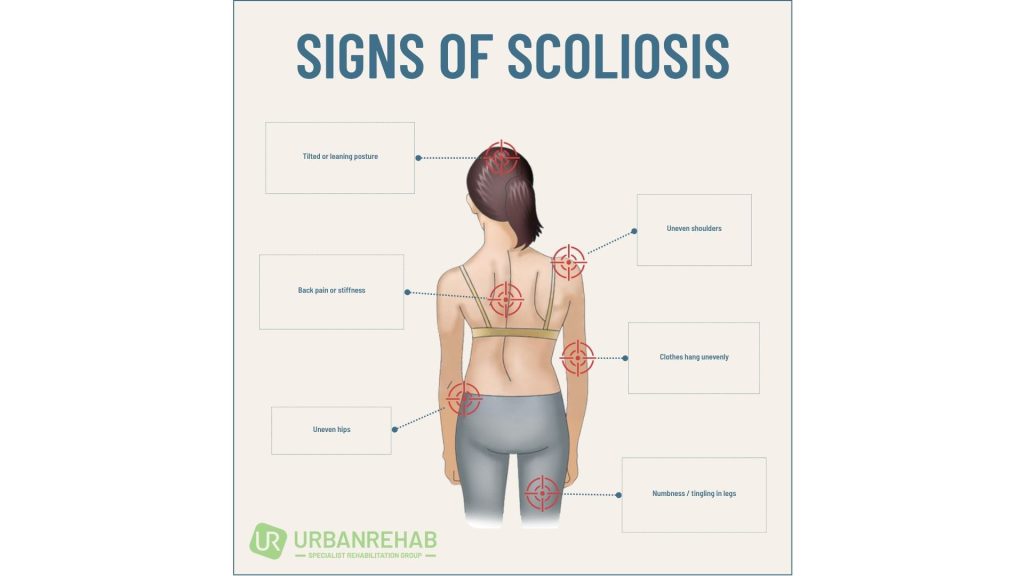
Common signs and symptoms include:
- Uneven shoulders or hips – one side appears higher than the other.
- Visible spinal curvature – a noticeable side-to-side curve in the spine.
- Lower back stiffness – especially after long periods of sitting or standing.
- Muscle fatigue and imbalance – soreness or tiredness in the back muscles due to uneven loading.
- Reduced flexibility – difficulty bending, twisting, or moving comfortably.
- Difficulty standing upright – a tendency to lean forward or issues with balance.
- General pain or discomfort – often due to strain on muscles and joints.
- Numbness or tingling in the legs – in cases where spinal nerves are compressed.
Can scoliosis be treated?
Yes – and early intervention is important. Most adults with scoliosis have a mild form of the condition that can be managed effectively without surgery. Conservative treatment options can reduce pain, improve function, and support better posture. These may include:
- Physiotherapy
- Acupuncture
- Massage therapy
- Ergonomic modifications at work or home
- Medication or nerve block injections for pain linked to arthritis or nerve compression
How physiotherapy can help
Physiotherapy plays a central role in the management of scoliosis – particularly for adults. Treatment plans are tailored to each individual and may involve:
- Postural retraining to correct alignment and reduce spinal strain
- Strengthening exercises focused on the core, back, and hips
- Manual therapy to relieve tightness and improve joint mobility
- Education on safe movement patterns, lifting strategies, and daily posture habits
- Pain management, including soft tissue release, acupuncture, or electrotherapy
These techniques aim to reduce discomfort, slow the progression of the spinal curve, and enhance quality of life – all through non-invasive care.
Can scoliosis be prevented?
While scoliosis itself is not preventable, there are steps you can take to minimise its progression and protect your spine as you age:
- Stay physically active
- Maintain muscle strength and flexibility
- Support bone health, especially during and after menopause
- Seek early intervention if you notice changes in your posture or back pain
If you’re noticing signs of scoliosis or simply want to take better care of your spine as you age, our physiotherapy team is here to help. We’ll work with you to create a personalised plan that supports mobility, comfort, and long-term spinal health.
Book your appointment here
Your spine supports you every day – let’s help it stay strong for life.
Written By Lisa Gold, Principal Physiotherapist, Urban Rehab