A TPA That Cares for People, Not Just Claims
Because managing employee health benefits should be simple, transparent, and human.
A TPA That Cares for People, Not Just Claims
Because managing employee health benefits should be simple, transparent, and human.
At Fullerton Health Singapore, we believe in simplifying employee healthcare management with trusted expertise and technology.
Our Third-Party Administrator (TPA) services make it easier for organisations to care for their teams with confidence. We bring together technology, a reliable healthcare network, and dedicated support to ensure every employee feels supported from claim to recovery.
It’s an approach built around people, not processes — where every claim is handled with accuracy, care, and respect.
Third-Party Administrator (TPA) Services in Singapore
A Third-Party Administrator (TPA) acts as the link between insurers, employers, and healthcare providers, handling the day-to-day administration of employee health benefits so organisations can focus on their people.
At Fullerton Health, this function sits within our Medical Benefits Management Services (MBMS) department, reflecting a more holistic approach to benefits processing, where administrative accuracy is strengthened with medical understanding.
Our services include:
Receiving, verifying, and adjudicating claims
Facilitating cashless hospitalisation between patients and healthcare providers
Providing reports and analytics to stakeholders
Comprehensive TPA Solutions for Corporates
With decades of regional experience in healthcare management, Fullerton Health Singapore provides Third-Party Administrator (TPA) services built on precision, transparency, and care.
Our approach combines technology with trusted human support, ensuring every claim, report, and interaction is handled with accuracy and empathy.
Smart, Secure, and Seamless Claims Management
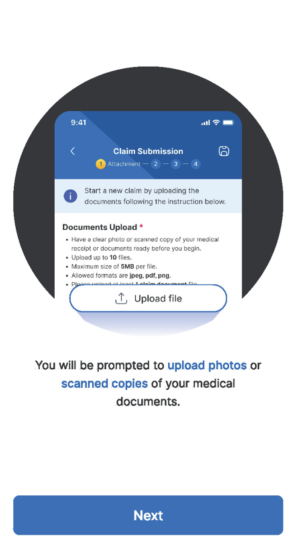
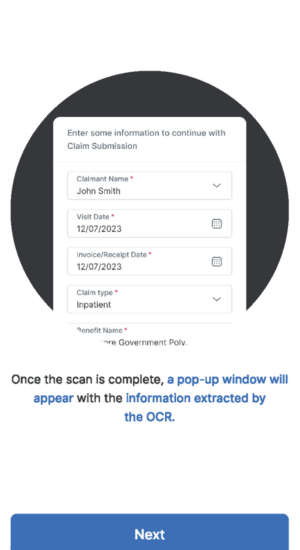
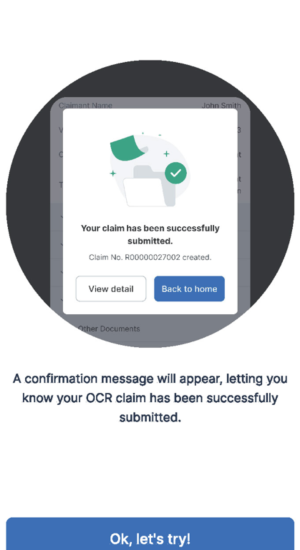
- Automated verification and processing through AI/OCR-enabled systems for faster turnaround and fewer errors.
- Robust data privacy and protection built on SOC2-certified information security standards.
- Continuous optimisation to maintain the highest levels of speed, accuracy, and compliance.
Dedicated Support, Every Step of the Way
Our experienced support team and dedicated hotline provide timely, empathetic assistance for members and corporate partners. Every interaction reflects our commitment to making healthcare administration simple, responsive, and human.
Cashless Access Islandwide
- Leverage our extensive network of 1000+ Fullerton Health clinics and partner medical facilities islandwide.
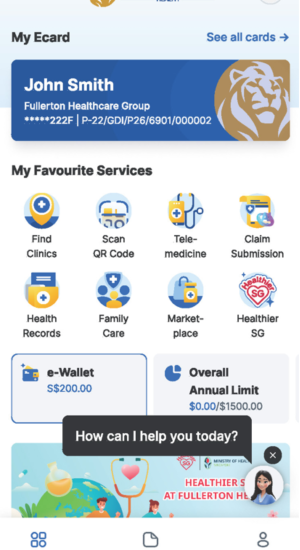
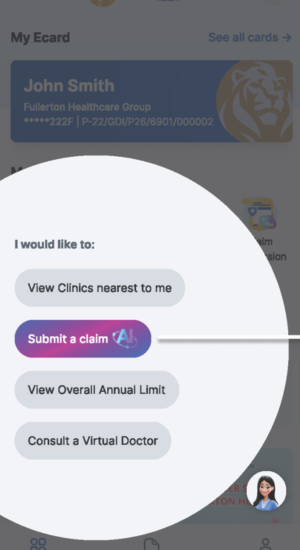
- Integrated via the Fullerton Health Concierge app, enabling members to submit and track claims, view benefits, and access telemedicine services all on one platform.
Actionable Insights for Smarter Decisions
- Comprehensive analytics and extensive report templates for insurers, brokers, and HR teams.
- Access to cost summaries, utilisation trends, and claims data for better planning and budgeting.
- Transparent insights that help employers and partners make informed, strategic decisions about workforce health.
The Fullerton Health Difference
At Fullerton Health Singapore, we understand the expectations of both employers and employees.
Partnering with Fullerton Health means having a TPA that:
Understands Local Needs
Deep understanding of Singapore’s corporate healthcare landscape and unique requirements.
Reliable Technology
Cutting-edge systems ensuring operational excellence and seamless service delivery.
Service Quality First
We value service quality as much as efficiency, ensuring every interaction matters.
Ready to simplify your employee healthcare management?
Get in touch with our Medical Benefits & Management Services team
today to learn more about our TPA solutions:




